
Most SVTs depend on the AV node for maintenance of the re-entry circuit and can be interrupted by (vagal) maneuvers or pharmacological agents, which slow AV nodal conduction, the first-line pharmacological agent being adenosine. After restoration of sinus rhythm, the twelve-lead ECG should be examined for the presence of delta waves, which indicate an accessory pathway. The usual electrocardiographic presentation of SVT is a narrow complex tachycardia (QRS less than 120ms), but in some cases (less than 10%), SVT presents as wide complex tachycardia. SVTs are often recurrent, occasionally persistent, and are a frequent cause of emergency room (ER) and primary care physician (PCP) visits. Syncope is uncommon, but some patients experience serious psychologic distress.
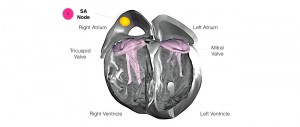
Tachycardias can be categorized as ventricular (involving the ventricle ± the His-Purkinje system) and supraventricular (all the others arrhythmias).
Atrial flutter ablation indications update#
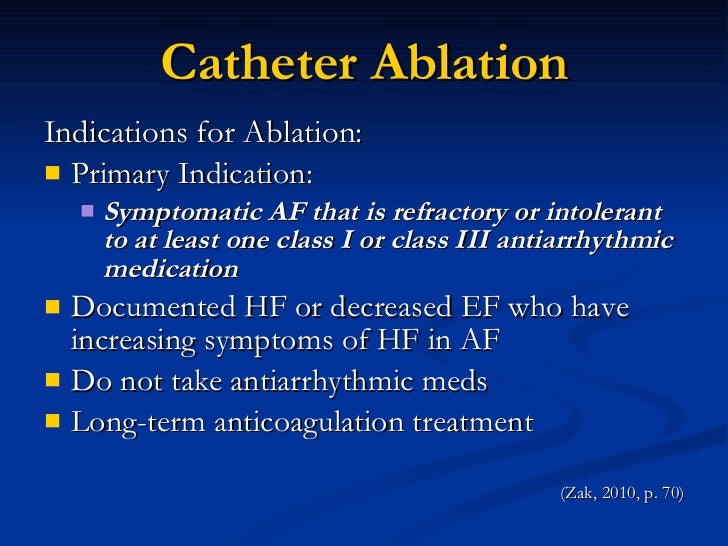
Catheter ablation of SVT has emerged as a curative treatment with high success rates and plays a central role in the management of supraventricular tachycardia (SVT).This short review aims to give an update on the outcomes of catheter ablation and provide a guide to appropriate decision making in patients with SVT.


 0 kommentar(er)
0 kommentar(er)
